- All Locations
- New York
- Amherst
uBreakiFix - Phone and Computer Repair - Amherst
uBreakiFix - Phone and Computer Repair - Amherst
Same-day repairs
Quality parts and upgrades
We fix anything with a power button
Select a device to get started.
Have a protection plan? Start a claim.

uBreakiFix—now by Asurion
uBreakiFix® and Asurion are now uBreakiFix by Asurion, providing even better service along with the same great quality repairs.
We fix phones, computers, tablets, game consoles, and more
Have your Google Pixel™ put back in one piece by an authorized repair provider
Schedule a repairSchedule a repair
Not sure what’s wrong? Let us take a look.

Speedy service
Most repairs done in 45 minutes or less.

We'll beat any local competitor’s published price for the same repair by $5.

Most repairs come with our hassle-free warranty—valid at any location.
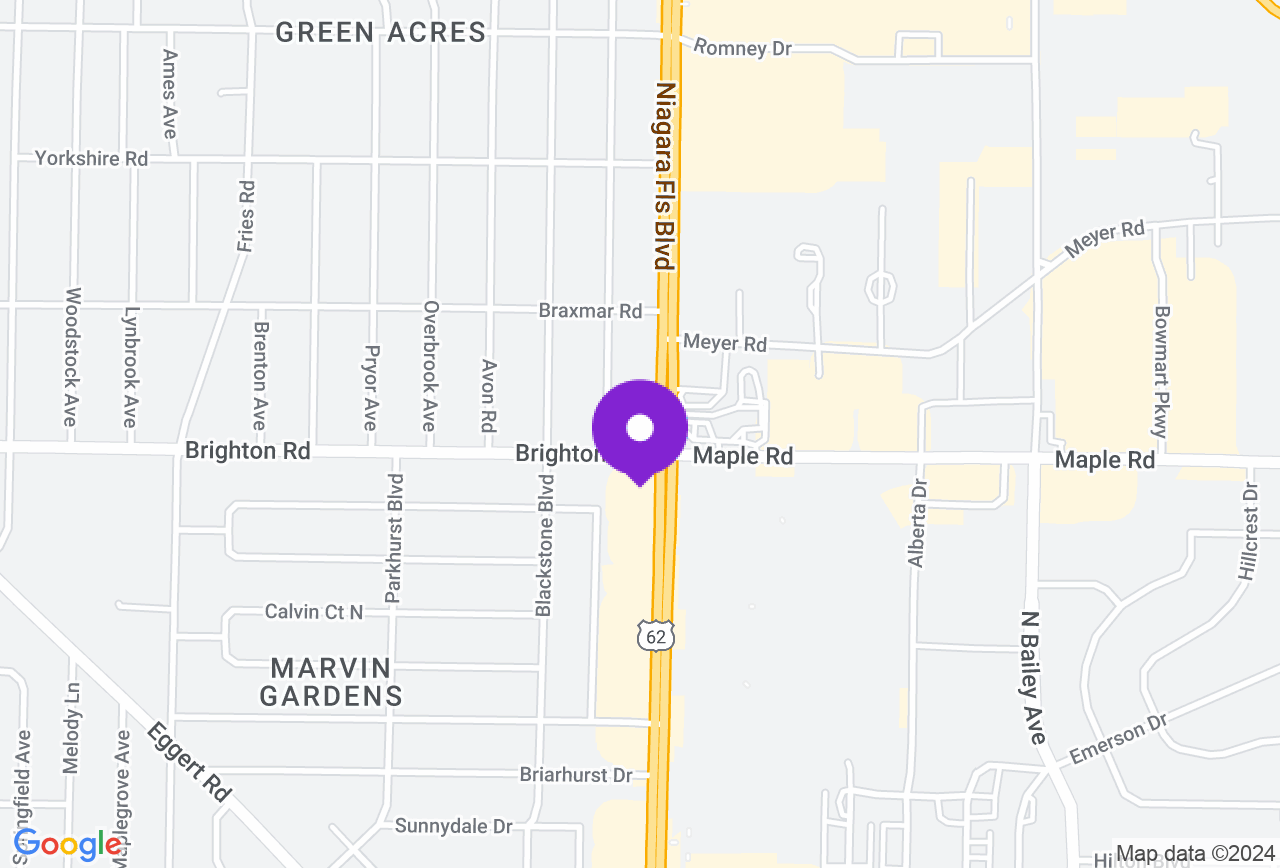
Visit our Amherst store

Stop by our Tonawanda, NY store, and one of our experts will fix your tech with or without an appointment. Can’t come in? We have mobile repair vans that’ll come to you.

The team at our Tonawanda, NY store can repair your devices and resolve your tech problems too. Not sure what’s wrong with your device? We'll run a free diagnostic.

When customers visit our Tonawanda, NY store, they receive fast, affordable repairs—most repairs done in 45 minutes or less, and come with our hassle-free 1-year limited warranty.
What our Amherst customers are saying
OUT OF 485 REVIEWS
4.6
STAR RATING
Whether you had a stellar experience or you think there’s room for improvement, please let us know. We value your experience at our stores above anything else. We want to hear from you!
Shelley E
08/28/2024
Samsung Galaxy S24 Repair | Amherst
Raymond N
08/24/2024
PC Repair | Amherst
Andrea D
08/20/2024
iPhone 12 Repair | Amherst
What can we fix for you today?

Have old devices? Bring them in.
We partner with Samsung to securely and responsibly recycle tech.Learn More
Your tech. Fixed.
We repair the devices you rely on most. Here are some of the issues we can help resolve:
Electronics, phone, and computer repair in Tonawanda, NY at uBreakiFix® by Asurion
Want a fix for your broken tech? Looking for a fast screen repair near you? For the best phone, electronics, and computer repair in Tonawanda, visit your local uBreakiFix by Asurion store. Our friendly experts are highly skilled and here to help. We offer phone repair, like screen replacements for iPhone® devices or Samsung Galaxy battery replacements, tablet repairs for devices like Surface Pro® tablets, PC or laptop repairs for everything from Dell® to Lenovo®, game console repairs for your Nintendo Switch™, PlayStation®, or Xbox®, and answers for a plethora of other electronics, too.
Certified pros and no-cost diagnostics
uBreakiFix by Asurion stores offer a 0 dollar diagnostic for full transparency throughout the repair process. Whether you try our mail-in services, book an appointment online, or simply walk in, trust our certified professionals for the best fix in town. Before your repair, we also offer an up-front diagnostic report and repair estimate, whether you opt for an iPhone screen replacement, iPad repair, or another fix—and our price-match guarantee means we’ll be happy to meet any regularly published local competitor's price for the same repair, then drop it by another $5.*
The top phone repair in Tonawanda
At our stores, we complete every repair with quality components made to the exact original equipment manufacturer (OEM) specifications. We partner proudly with Google® and Samsung® as an authorized service provider, including for our tablet repair and phone repair services. uBreakiFix by Asurion Experts use replacement parts that are tested regularly to ensure quality, and our staff prides themselves on providing an easy repair experience for everyone who comes to our store for help.
Fix the tech you love
You depend on your computer, phone, or tablet to catch flicks, chat with friends, or finish your work. When it isn’t working the way it should, you need to find a fix fast. That's why we’re here to help get your tech working again quickly. Many simpler tablet or phone repair services are completed the same day, often within 2 hours or less. Phone battery repair, tablet screen replacements, computer virus removal: uBreakiFix by Asurion Experts can tackle it all, having completed more than 14 million repairs to date. Consider us your full-service shop for everything electronics repair related in Tonawanda.
Computer repair in Tonawanda, NY
With a local uBreakiFix by Asurion store, getting a computer repair in Tonawanda is simple. Wondering how you can get the power button fixed on your PC, like a Lenovo® or MacBook® laptop? We cover fixes ranging from MacBook repair to Alienware updates. Our team works tirelessly to make your fix process effortless and easy, and we provide a 1-year limited warranty for our repairs. If you've been looking online for a "computer repair near me," you've come to the right place. uBreakiFix by Asurion Experts offer a personalized repair experience to make sure your computer repair services are completed on time and your tech is returned to you in top shape.
We fix virtually everything with a power button. Bring your broken tech to the local pros today.
** Our repairs come with a 1-year limited warranty, valid at all our locations. The only exceptions are liquid damage repairs or if we’re working on your device through your Original Equipment Manufacturer warranty or some other coverage plan. Then the terms of that coverage would apply.