Authorized to fix your device
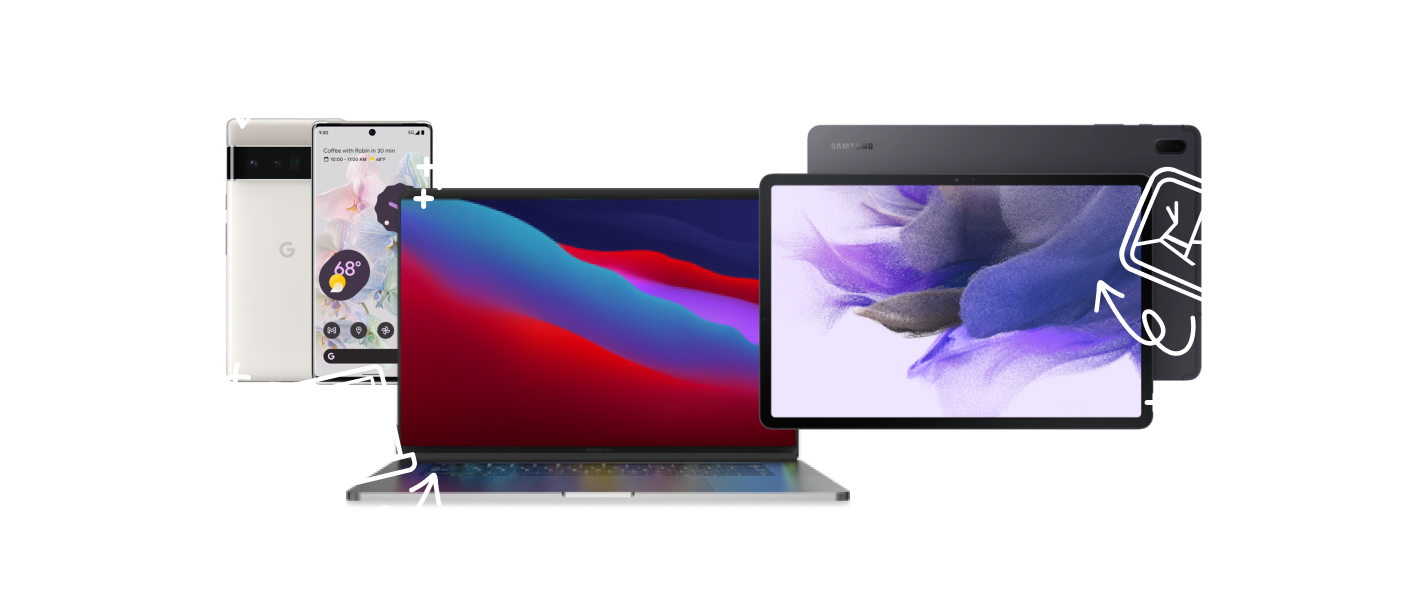
As an authorized Samsung® and Google® repair provider, and Independent Repair Provider for Apple®, we’ll only use parts, tools, and equipment that meet their standards. So don’t leave important repairs to just anyone. Ours are done right.
Our Tablet Wi-Fi repairs are simple

2. Get quality repairs
We’ll run a free diagnostic on your Tablet and provide fast, convenient repairs.

3. Sit back and relax
We’ll contact you when the repair is done so you can enjoy your Tablet.

Quality repairs, right in your neighborhood
Trusted professionals. 700+ locations and thousands of experts.
Speedy service. Most repairs done as soon as same day.
Free diagnostics. Not sure what’s wrong? Let us take a look.
Low prices. We’ll beat any local competitor’s price.
1-year limited warranty. It comes standard with most of our repairs.
Your Tablet is in good hands
Don’t leave important repairs to just anyone. For over 25 years, Asurion has repaired the devices people rely on most. And we have the reviews to prove it.
Tablet WiFi and BlueTooth issues at uBreakiFix® by Asurion
uBreakiFix® by Asurion store experts provide world-class, professional tablet WiFi and BlueTooth issues services at an affordable price, so you can get back to your life quickly. We also include a complimentary diagnostic and service estimate upfront, so there are no hidden fees when the bill comes. With 700+ stores to choose from, uBreakiFix by Asurion offers fast, trustworthy tech services right in your neighborhood. In select areas, we can even come to you for certain repairs—fixing tech from almost anywhere.
How much are your tablet WiFi or BlueTooth services?
We ensure all of our services are available for a competitive rate without forfeiting quality, including tablet wifi repairs. As an Independent Repair Provider for Apple® devices, and an authorized repair provider for Google® and Samsung® , we expedite our repair process and pass savings along to the people we serve—while ensuring our parts are high quality, made to the original manufacturer’s exact standards. Found a better deal online? We’ll meet any local competitor’s regularly published price for the same service, then we’ll beat it by $5. We also provide a 1-year limited warranty on our work,* so if the same issue we serviced reoccurs—you're covered.
How fast are your tablet WiFi repair services?
Our experts can usually complete tablet WiFi repair services or Bluetooth tablet repairs the day you bring in your device. If your tablet needs a simple repair, we're able to complete some in just a few hours. Tech is important to us, too, so we know how critical your devices are for staying connected to those you love. If our experts are busier than usual, we’ll keep you updated when it comes to the status of your repair or service so you can plan accordingly.
Why is my tablet not connecting to Wi-Fi?
There's a number of potential reasons a tablet won't connect to WiFi. To find out exactly what the issue is, bring your tech to the closest uBreakiFix by Asurion for a free diagnostic from pros. Our technicians are required to finish a comprehensive training program—making them some of the best in the industry. They have already helped with over 15 million repairs, and they can't wait to help you. We believe people should never face the difficult decision of sacrificing quality for affordability. You can count on us to get your tablet WiFi or BlueTooth issues completed quickly at a price that won't break the bank.
We make Tablet Wi-Fi repairs easy

Stop by your local store, and one of our experts will fix your Tablet with or without an appointment. Can’t come in? We have mobile repair vans that’ll come to you in select cities.

The team at your local store can repair your Tablet and resolve your tech problems too. Not sure what’s wrong with your device? We’ll diagnose it for free.

When customers visit our store, they receive fast, affordable tech repairs—many completed as soon as the same day. And most of those repairs come with a 1-year limited warranty.
What else can we fix for you?
The Asurion® trademarks and logos and the uBreakiFix® trademarks and logos are the property of Asurion, LLC and uBreakiFix Co. respectively. All rights reserved. All other trademarks are the property of their respective owners. Asurion and uBreakiFix are not affiliated with, sponsored by, or endorsed by any of the respective owners of the other trademarks appearing herein.
Apple, iPhone and iPad are trademarks of Apple, Inc. All other trademarks are the property of their respective owners. Asurion is not affiliated with, sponsored by, or endorsed by Apple or any of the respective owners of the other trademarks appearing herein.
























